Sexual Loneliness and Its Impact on Intimate Health: A Comprehensive Approach to Social Isolation Challenges

Sexual loneliness represents an increasingly prevalent yet underrecognized public health challenge with profound implications for individual wellbeing and societal health outcomes. This comprehensive analysis examines the multifaceted nature of sexual loneliness as distinct from general loneliness, exploring its complex etiology, physiological and psychological manifestations, and far-reaching consequences for intimate health. Through systematic examination of contemporary research, clinical observations, and epidemiological data, this review elucidates the bidirectional relationship between sexual loneliness and various health domains, including cardiovascular function, immune system integrity, mental health stability, and overall quality of life. The investigation reveals significant gender disparities in both prevalence and manifestation patterns, with particular attention to the emerging crisis among young adults. This work provides evidence-based therapeutic frameworks and preventive strategies while addressing the sociocultural factors that contribute to the escalation of sexual loneliness in modern society. The findings underscore the urgent need for healthcare professionals to recognize sexual loneliness as a legitimate clinical concern requiring specialized intervention approaches that integrate psychological, social, and medical perspectives.
Introduction
The human need for intimate connection extends far beyond mere companionship, encompassing complex psychological, physiological, and social dimensions that fundamentally influence health and wellbeing. Sexual loneliness, defined as the subjective distress arising from the absence of desired sexual and romantic connections, represents a distinct phenomenon that differs qualitatively from general social loneliness. While social loneliness may be ameliorated through various forms of human contact, sexual loneliness specifically relates to the deficit in intimate, romantic, and sexual relationships that fulfill fundamental human needs for physical closeness, emotional intimacy, and sexual expression.
Recent epidemiological evidence reveals a concerning trend in the prevalence of sexual loneliness, particularly among younger demographics. Contemporary societal changes, including technological disruption of traditional relationship formation patterns, economic pressures extending dependency periods, and evolving cultural attitudes toward intimacy and commitment, have created unprecedented challenges for intimate relationship development. These changes have coincided with documented increases in sexual inactivity among young adults, creating what some researchers characterize as an emerging public health crisis.
The significance of sexual loneliness extends beyond individual suffering to encompass broader societal implications. Research demonstrates that the absence of intimate relationships correlates with increased healthcare utilization, reduced productivity, and elevated risk for various physical and mental health conditions. The economic burden associated with these outcomes, combined with potential social stability implications, positions sexual loneliness as a critical area for public health intervention and clinical attention.
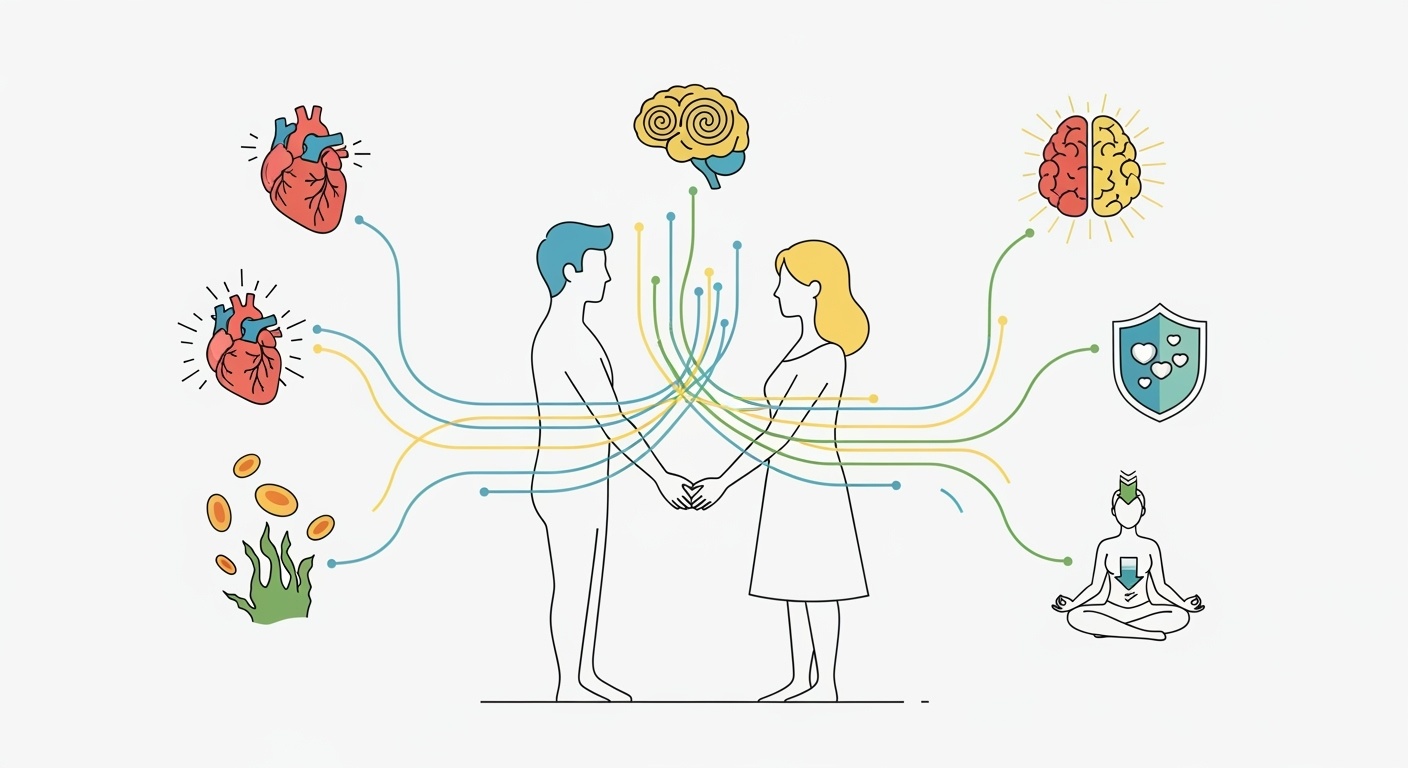
Understanding sexual loneliness requires recognition of its multidimensional nature, encompassing physical, emotional, and social components that interact in complex ways. The physical aspects involve the absence of sexual activity and physical intimacy, while emotional dimensions include the lack of romantic connection, emotional support, and partnership. Social elements encompass feelings of exclusion from couple-oriented social activities and the absence of a primary relationship that provides social identity and belonging.
Conceptual Framework and Definitions
Sexual loneliness represents a complex psychosocial phenomenon that requires precise conceptualization to distinguish it from related but distinct constructs. At its core, sexual loneliness involves the subjective experience of distress resulting from the perceived discrepancy between desired and actual levels of intimate, romantic, and sexual connection. This definition encompasses both the quantitative aspect of relationship absence and the qualitative dimension of unmet intimacy needs, recognizing that individuals may experience sexual loneliness even within existing relationships if those relationships fail to provide adequate intimate connection.
The conceptual framework for understanding sexual loneliness incorporates multiple theoretical perspectives, drawing from attachment theory, social exchange theory, and evolutionary psychology. Attachment theory provides insight into how early relational experiences shape adult intimacy patterns and vulnerability to sexual loneliness. Individuals with insecure attachment styles may experience greater difficulty forming intimate relationships and heightened distress when relationships are absent or unsatisfying. Social exchange theory illuminates the cost-benefit analyses individuals perform when seeking relationships, highlighting how perceived barriers to relationship formation may contribute to prolonged periods of sexual loneliness.
Evolutionary psychology offers additional perspective on sexual loneliness by positioning intimate relationships within the context of fundamental human survival and reproductive strategies. From this viewpoint, sexual loneliness represents a deviation from evolutionarily adaptive patterns of pair bonding and mating, potentially triggering stress responses that served protective functions in ancestral environments but may prove maladaptive in contemporary contexts.
The multidimensional nature of sexual loneliness encompasses several distinct but interrelated components. Emotional intimacy involves the capacity for deep emotional connection, vulnerability sharing, and mutual understanding within romantic relationships. Physical intimacy encompasses both sexual activity and non-sexual physical affection, including touch, cuddling, and other forms of physical closeness. Social intimacy relates to shared activities, mutual interests, and the companionship aspects of romantic partnerships. Existential intimacy involves the sense of meaning and purpose derived from committed relationships and the shared life narratives that develop within partnerships.
Sexual loneliness differs from sexual dysfunction in that it primarily concerns relationship absence rather than performance difficulties within existing relationships. However, the two phenomena may interact, as sexual loneliness can contribute to performance anxiety when opportunities for intimacy arise, while sexual dysfunction can contribute to relationship dissolution and subsequent sexual loneliness. Understanding these distinctions proves crucial for appropriate clinical assessment and intervention planning.
Epidemiological Trends and Demographics
Contemporary demographic analysis reveals alarming trends in the prevalence of sexual loneliness across various population segments, with particularly concerning patterns emerging among young adults. National survey data consistently demonstrates increasing rates of sexual inactivity among individuals aged eighteen to twenty-four, with some studies indicating that nearly one-third of young men in this age group report no sexual activity within the past year. This represents a substantial increase from previous decades and suggests a fundamental shift in young adult relationship patterns.
Gender disparities in sexual loneliness prevalence reflect complex interactions between biological, psychological, and social factors. Research indicates that men experience higher rates of complete sexual inactivity, while women more commonly report dissatisfaction with the quality rather than quantity of intimate relationships. These differences may reflect varying cultural expectations regarding relationship initiation, different approaches to sexual satisfaction, and distinct patterns of emotional expression and intimacy needs.
Age-related patterns in sexual loneliness reveal concerning trends across the lifespan. While young adults show increasing rates of sexual inactivity, middle-aged individuals demonstrate growing prevalence of sexual loneliness within marriages and long-term partnerships. Older adults face unique challenges related to partner loss, health changes, and ageist attitudes that may limit relationship opportunities. Each age group presents distinct clinical considerations and intervention needs.
Socioeconomic factors significantly influence sexual loneliness prevalence and manifestation. Economic instability, extended educational periods, and changing career patterns have delayed traditional relationship milestones for many individuals. Lower socioeconomic status correlates with increased sexual loneliness rates, possibly reflecting reduced relationship opportunities, increased stress levels, and limited access to mental health resources that might address underlying contributors.
Cultural and ethnic variations in sexual loneliness patterns reflect different relationship norms, family structures, and community support systems. Some cultural groups demonstrate resilience factors that appear protective against sexual loneliness, including extended family involvement in relationship formation, community-based social activities, and cultural emphasis on interdependence rather than individual achievement.
Geographic factors also influence sexual loneliness prevalence, with urban and rural environments presenting different challenges and opportunities for relationship formation. Urban areas may offer greater relationship diversity but also increased competition and social fragmentation. Rural communities may provide stronger social cohesion but limited relationship options, particularly for individuals with minority identities or non-traditional relationship preferences.
Physiological Impact and Health Consequences
The physiological consequences of sexual loneliness extend far beyond the obvious absence of sexual activity, encompassing complex neuroendocrine, immune, and cardiovascular effects that significantly impact overall health. Research demonstrates that intimate relationships provide measurable physiological benefits through multiple biological pathways, and the absence of these relationships correspondingly produces detectable negative health outcomes.
Neuroendocrine research reveals that sexual loneliness disrupts normal hormonal patterns in ways that affect both physical and mental health. Chronic loneliness states activate the hypothalamic-pituitary-adrenal axis, leading to elevated cortisol levels that, when sustained, contribute to immune suppression, increased inflammation, and metabolic dysfunction. Conversely, satisfying intimate relationships promote the release of oxytocin, vasopressin, and other hormones associated with pair bonding, stress reduction, and overall wellbeing.
The cardiovascular implications of sexual loneliness prove particularly significant, with research demonstrating increased risk for hypertension, coronary artery disease, and stroke among chronically lonely individuals. The mechanisms underlying these relationships involve both direct physiological effects of chronic stress and indirect effects through health behaviors. Sexual loneliness may contribute to cardiovascular risk through elevated baseline cortisol levels, increased inflammatory markers, and disrupted circadian rhythms that affect cardiovascular function.
Immune system function shows marked differences between individuals with satisfying intimate relationships and those experiencing sexual loneliness. Chronic loneliness correlates with increased susceptibility to viral infections, delayed wound healing, and elevated markers of systemic inflammation. The immune changes associated with sexual loneliness may reflect evolutionary adaptations to social isolation that become maladaptive in modern contexts where isolation does not necessarily indicate immediate physical threat.
Sleep disturbances frequently accompany sexual loneliness, creating cascading effects on multiple physiological systems. The absence of a sleeping partner eliminates various sleep-promoting factors, including shared body heat, consistent sleep schedules, and the security associated with companionship. Sexual loneliness may also contribute to rumination and anxiety that directly interfere with sleep quality, creating cycles of sleep disruption that further compromise physical and mental health.
Pain perception and management show interesting relationships with sexual loneliness, as intimate relationships provide multiple mechanisms for pain relief, including physical comfort, emotional support, and distraction from discomfort. The absence of these natural pain management resources may contribute to increased pain sensitivity and reduced pain tolerance among sexually lonely individuals. This relationship proves particularly relevant for chronic pain conditions that may be exacerbated by the absence of intimate support.
Metabolic effects of sexual loneliness include increased risk for obesity, diabetes, and metabolic syndrome. These relationships may reflect both direct hormonal effects of chronic stress and indirect effects through comfort eating, reduced motivation for self-care, and decreased participation in physical activities that might occur within romantic partnerships. The metabolic consequences of sexual loneliness represent important considerations for comprehensive health management.
Psychological and Emotional Manifestations
The psychological impact of sexual loneliness encompasses a broad spectrum of emotional, cognitive, and behavioral manifestations that significantly affect quality of life and functional capacity. Unlike temporary loneliness that may resolve with general social contact, sexual loneliness often persists despite adequate social connections in other domains, creating unique psychological challenges that require specialized understanding and intervention approaches.
Depression represents one of the most common psychological consequences of sexual loneliness, with research demonstrating bidirectional relationships between depressive symptoms and relationship difficulties. Sexual loneliness may contribute to depression through multiple pathways, including reduced self-esteem, hopelessness about future relationship prospects, and the absence of intimate support that typically provides resilience against depressive episodes. The specific type of depression associated with sexual loneliness often includes themes of unworthiness, social inadequacy, and existential emptiness that general antidepressant treatments may not fully address.
Anxiety manifestations in sexual loneliness frequently center on social and performance concerns that create self-perpetuating cycles of avoidance and increased isolation. Social anxiety may develop or intensify in response to repeated relationship disappointments, creating barriers to future relationship attempts. Performance anxiety regarding sexual activity may emerge after extended periods of sexual inactivity, further complicating relationship formation when opportunities arise. These anxiety patterns require careful assessment to distinguish between primary anxiety disorders and secondary anxiety resulting from sexual loneliness.
Self-esteem and identity issues prove particularly complex in sexual loneliness, as intimate relationships typically provide important sources of validation, identity confirmation, and self-worth. The absence of romantic relationships may lead individuals to question their desirability, competence, and fundamental worth as human beings. These self-concept disturbances often extend beyond romantic contexts to affect professional performance, social relationships, and general life satisfaction.
Cognitive distortions commonly develop in response to prolonged sexual loneliness, including catastrophic thinking about relationship prospects, overgeneralization from negative relationship experiences, and dichotomous thinking about relationship success and failure. These cognitive patterns may contribute to unrealistic relationship expectations, premature relationship termination, or excessive tolerance for unsatisfying relationships based on fear of returning to loneliness.
Emotional regulation difficulties frequently accompany sexual loneliness, as intimate relationships typically provide crucial support for emotional processing and regulation. Without a primary relationship partner to share emotional experiences, individuals may struggle with emotional overwhelm, difficulty processing complex feelings, and reduced emotional intelligence development. These regulatory challenges may affect all life domains, not solely romantic relationships.
Behavioral manifestations of sexual loneliness vary considerably among individuals but commonly include social withdrawal, compulsive behaviors, and maladaptive coping strategies. Some individuals respond to sexual loneliness through increased social activity and relationship seeking, while others withdraw from social contact to avoid reminders of their relationship status. Compulsive behaviors, including excessive use of pornography, serial casual relationships, or obsessive focus on appearance and attractiveness, may represent attempts to address sexual loneliness that ultimately prove counterproductive.
The temporal aspects of psychological responses to sexual loneliness prove important for understanding individual variation in coping and adaptation. Acute responses to relationship loss or prolonged singleness may differ significantly from chronic adaptation patterns that develop over extended periods. Some individuals demonstrate remarkable resilience and adaptation to single life, while others experience progressive deterioration in psychological functioning with extended periods of sexual loneliness.
Gender Differences and Disparities
Gender differences in sexual loneliness prevalence, manifestation, and consequences reflect complex interactions between biological factors, social conditioning, and cultural expectations that require nuanced understanding for effective clinical intervention. Research consistently demonstrates that men and women experience sexual loneliness differently, with distinct patterns of onset, symptom presentation, and coping strategies that necessitate gender-informed approaches to assessment and treatment.
Men demonstrate higher rates of complete sexual inactivity and report greater distress specifically related to the absence of sexual activity. This pattern may reflect biological differences in sexual motivation, social conditioning regarding male sexual initiative, and cultural expectations that position sexual success as integral to masculine identity. Male sexual loneliness often presents with themes of failure, inadequacy, and social rejection that may be particularly devastating given cultural messages about male sexual competence and relationship responsibility.
The psychological manifestations of sexual loneliness in men frequently include anger, resentment, and externalization of blame that may be directed toward potential partners, society, or cultural changes perceived as creating barriers to relationship formation. These responses may reflect socialization patterns that discourage emotional vulnerability and promote external attribution for personal difficulties. Male sexual loneliness may also manifest through increased risk-taking behaviors, substance use, and aggressive tendencies that represent maladaptive attempts to address underlying emotional needs.
Women experiencing sexual loneliness more commonly report dissatisfaction with relationship quality rather than complete absence of romantic connections. Female sexual loneliness often centers on themes of emotional intimacy, relationship depth, and partner emotional availability rather than purely physical concerns. This pattern may reflect socialization emphasizing emotional connection, cultural permission for women to prioritize relationship quality over quantity, and different approaches to sexual satisfaction that emphasize emotional context.
The coping strategies employed by women experiencing sexual loneliness frequently involve increased social connection, self-improvement activities, and meaning-making through alternative life domains such as career, friendships, or creative pursuits. Women may demonstrate greater resilience to sexual loneliness through stronger social support networks and cultural acceptance of single life as potentially fulfilling and meaningful.
Biological factors contribute to gender differences in sexual loneliness through hormonal influences on sexual motivation, attachment behaviors, and stress responses. Testosterone levels affect sexual desire and motivation in complex ways that may influence male experiences of sexual loneliness. Estrogen and progesterone fluctuations affect female emotional states and relationship priorities in patterns that may influence sexual loneliness manifestation and timing.
Cultural factors significantly shape gender differences in sexual loneliness through differential socialization regarding relationship roles, sexual expression, and emotional communication. Traditional gender roles that position men as relationship initiators may create particular vulnerability to sexual loneliness when social skills or confidence are limited. Cultural messages about female sexual selectivity may contribute to different relationship strategies that affect sexual loneliness patterns.
The intersection of gender with other identity factors, including sexual orientation, cultural background, and socioeconomic status, creates additional complexity in sexual loneliness patterns. Sexual minority individuals may face unique challenges related to limited relationship pools, social stigma, and identity development processes that affect sexual loneliness experiences. Understanding these intersectional factors proves crucial for comprehensive assessment and culturally competent intervention.
Age-related gender differences in sexual loneliness reveal changing patterns across the lifespan that reflect biological, psychological, and social developmental processes. Young adult gender differences may reflect different approaches to relationship formation and sexual exploration. Middle-aged patterns may be influenced by parenting demands, career pressures, and changing relationship priorities. Older adult gender differences often reflect different patterns of partner loss, health changes, and social expectations regarding late-life sexuality.
Social and Cultural Factors
The contemporary landscape of sexual loneliness cannot be understood without examining the profound social and cultural transformations that have reshaped relationship formation, maintenance, and dissolution patterns over recent decades. These changes have created unprecedented challenges for intimate connection while simultaneously altering social expectations and support systems that traditionally facilitated relationship development.
Technological disruption of traditional relationship formation represents one of the most significant cultural factors influencing sexual loneliness prevalence. Digital communication platforms, social media, and dating applications have fundamentally altered how individuals meet, interact, and develop intimate relationships. While these technologies ostensibly increase relationship opportunities, research suggests they may actually contribute to sexual loneliness through several mechanisms, including choice overload, commodification of relationships, and reduced investment in individual connections.
The phenomenon of “ghosting” and other digital relationship behaviors reflects broader cultural shifts toward decreased commitment and increased disposability in romantic relationships. These patterns may contribute to sexual loneliness by creating uncertainty, reducing trust in relationship stability, and encouraging protective emotional withdrawal that inhibits intimate connection development. The ease of ending digital relationships may reduce individuals’ motivation to work through relationship challenges that previously would have been resolved through communication and compromise.
Economic factors significantly influence contemporary sexual loneliness patterns through their effects on relationship timing, stability, and expectations. Extended educational periods, delayed career establishment, and increased housing costs have postponed traditional relationship milestones for many individuals. The economic necessity for dual-career relationships creates new stresses and complications that may affect relationship satisfaction and stability.
Cultural emphasis on individual achievement and self-actualization may inadvertently contribute to sexual loneliness by promoting values that conflict with relationship development and maintenance. The cultural message that individuals should prioritize personal goals over relationship needs may create internal conflicts that inhibit intimate connection. Additionally, unrealistic relationship expectations promoted by media portrayals may contribute to relationship dissatisfaction and premature relationship termination.
Social support network changes affect sexual loneliness through their influence on relationship formation opportunities and emotional support availability. Traditional community structures that facilitated relationship development, including religious organizations, neighborhood communities, and extended family involvement, have weakened in many contexts. The resulting social fragmentation may increase reliance on romantic relationships to meet social needs while simultaneously reducing opportunities to develop those relationships.
Gender role evolution creates both opportunities and challenges for intimate relationship development. While expanded gender role flexibility may benefit some individuals, the uncertainty and conflict surrounding changing expectations may create relationship difficulties for others. Traditional relationship scripts provided clear, if restrictive, guidelines for relationship development, and their absence may contribute to confusion and conflict in contemporary relationships.
Cultural attitudes toward sexuality and intimacy significantly influence sexual loneliness patterns through their effects on sexual expression, relationship expectations, and stigma associated with various relationship configurations. Cultures that maintain restrictive attitudes toward sexuality may contribute to sexual loneliness through limited opportunities for sexual expression and development. Conversely, cultures that commodify sexuality may reduce its intimate meaning and contribute to sexual loneliness despite high levels of sexual activity.
The intersection of global cultural influences with local relationship norms creates additional complexity in contemporary sexual loneliness patterns. Globalization exposes individuals to diverse relationship models and expectations that may conflict with local norms, creating internal tension and relationship confusion. Immigration and cultural transition experiences may particularly affect sexual loneliness through disruption of traditional relationship support systems and cultural identity conflicts.
Social media influences on sexual loneliness extend beyond direct relationship formation to include effects on self-esteem, social comparison, and relationship expectations. Curated presentations of others’ relationships may contribute to unrealistic expectations and dissatisfaction with available relationship options. Social media may also contribute to sexual loneliness through time displacement that reduces face-to-face social interaction opportunities.
Clinical Assessment and Diagnostic Considerations
Comprehensive clinical assessment of sexual loneliness requires multidimensional evaluation approaches that distinguish it from related conditions while identifying contributing factors, severity indicators, and treatment implications. Unlike many psychological conditions with established diagnostic criteria, sexual loneliness lacks standardized assessment protocols, necessitating careful clinical judgment and individualized evaluation strategies.
The initial assessment process should explore the phenomenology of sexual loneliness through detailed inquiry about the individual’s subjective experience, including onset patterns, duration, intensity, and specific manifestations. Clinicians must distinguish between acute sexual loneliness following relationship loss and chronic patterns that may reflect underlying psychological or social factors. The assessment should examine both quantitative aspects, such as duration of relationship absence, and qualitative dimensions, including satisfaction with previous relationships and current relationship desires.
Differential diagnosis proves crucial for appropriate treatment planning, as sexual loneliness may be confused with depression, anxiety disorders, social phobia, or personality disorders. While sexual loneliness frequently co-occurs with these conditions, it represents a distinct phenomenon that requires specific therapeutic attention. Clinicians should assess whether sexual loneliness represents a primary concern or a secondary consequence of other psychological difficulties.
The assessment of contributing factors should examine multiple domains, including individual psychological factors, social skills and opportunities, cultural and family background, and medical or psychiatric conditions that may affect relationship formation or maintenance. Individual factors might include attachment styles, self-esteem levels, social anxiety, and previous relationship trauma. Social factors encompass relationship opportunities, social support systems, and community integration.
Medical assessment components should evaluate physical health conditions that might contribute to sexual loneliness, including hormonal imbalances, chronic illnesses, medications with sexual side effects, and disabilities that may affect relationship opportunities. Sexual dysfunction assessment proves important, as performance concerns may contribute to relationship avoidance and subsequent sexual loneliness.
Psychological testing may provide valuable information about personality factors, attachment styles, depression and anxiety levels, and social functioning that influence sexual loneliness. Standardized instruments for assessing loneliness, relationship satisfaction, social skills, and sexual functioning may inform treatment planning. However, clinicians should recognize that existing loneliness measures may not capture the specific aspects of sexual loneliness that differ from general social loneliness.
The assessment should examine coping strategies and resources that individuals use to manage sexual loneliness, including both adaptive and maladaptive patterns. Adaptive strategies might include social engagement, self-development activities, and meaning-making through alternative life domains. Maladaptive patterns could include social isolation, substance use, compulsive sexual behaviors, or excessive relationship seeking that interferes with relationship development.
Cultural competence in assessment requires understanding how cultural background influences relationship expectations, expression of emotional distress, and help-seeking behaviors. Some cultures may discourage direct discussion of sexual concerns, requiring sensitive inquiry approaches. Cultural factors may also influence the meaning and acceptability of single status, affecting individual distress levels and treatment goals.
Risk assessment should examine potential complications of sexual loneliness, including suicidal ideation, aggressive behaviors, or unsafe sexual practices that might result from desperation for connection. While sexual loneliness rarely leads to imminent safety concerns, clinicians should be aware of situations where isolation and hopelessness might contribute to dangerous behaviors.
The assessment process should explore individual goals and preferences for treatment, recognizing that not all individuals experiencing sexual loneliness desire romantic relationships. Some may benefit from acceptance-based approaches that focus on life satisfaction despite relationship absence, while others may prefer interventions targeting relationship skill development and opportunities.
Therapeutic Interventions and Treatment Approaches
Evidence-based therapeutic interventions for sexual loneliness require integrative approaches that address the multifaceted nature of intimate relationship difficulties while recognizing individual differences in treatment needs and goals. Unlike standardized treatments for specific mental health conditions, sexual loneliness interventions must be tailored to individual circumstances, contributing factors, and personal preferences regarding relationship outcomes.
Cognitive-behavioral therapy represents a foundational approach for addressing sexual loneliness through its focus on identifying and modifying thought patterns and behaviors that contribute to relationship difficulties. CBT interventions for sexual loneliness typically target negative self-talk about desirability and relationship prospects, catastrophic thinking about relationship outcomes, and behavioral avoidance patterns that limit relationship opportunities. Specific techniques include cognitive restructuring to address distorted thinking about relationships, behavioral activation to increase social engagement, and exposure therapy to address social anxiety that may inhibit relationship formation.
The cognitive component of treatment addresses common thinking patterns associated with sexual loneliness, including all-or-nothing thinking about relationship success, personalization of relationship disappointments, and fortune-telling about future relationship prospects. Clients learn to identify these cognitive distortions and develop more balanced, realistic perspectives about relationships and their own relationship potential. Cognitive work also addresses beliefs about relationships, including unrealistic expectations and fears about vulnerability and intimacy.
Behavioral interventions focus on increasing activities and behaviors that enhance relationship opportunities while developing social and relationship skills. These may include structured social activities, communication skills training, and gradual exposure to relationship-relevant situations. Behavioral assignments might involve joining social groups, practicing conversation skills, or engaging in activities that align with personal interests and values while providing opportunities to meet compatible individuals.
Mindfulness-based interventions offer valuable approaches for managing the emotional distress associated with sexual loneliness while developing acceptance and present-moment awareness that can improve relationship satisfaction when opportunities arise. Mindfulness techniques help individuals observe their loneliness-related thoughts and feelings without becoming overwhelmed by them, reducing reactivity and improving emotional regulation. These skills prove particularly valuable for managing anxiety about relationship outcomes and developing patience with the relationship development process.
Acceptance and Commitment Therapy provides a framework for helping individuals clarify their values regarding relationships while developing psychological flexibility in pursuing those values. ACT approaches recognize that some individuals may benefit from accepting single status while pursuing meaningful life activities, while others may choose to actively pursue romantic relationships. The therapy focuses on committed action toward valued life directions rather than solely on relationship outcomes.
Interpersonal therapy addresses relationship patterns and social skills that may contribute to sexual loneliness. IPT focuses on improving communication skills, resolving interpersonal conflicts, and processing relationship losses that may affect current relationship capacity. The therapy examines how past relationship experiences influence current relationship approaches and helps individuals develop healthier relationship patterns.
Attachment-based therapies prove particularly relevant for individuals whose sexual loneliness relates to early attachment experiences that affect adult relationship capacity. These approaches help individuals understand how childhood experiences with caregivers influence current relationship expectations, fears, and behaviors. Attachment-focused interventions may involve processing early relationship trauma, developing secure attachment behaviors, and healing attachment wounds that interfere with intimate connection.
Group therapy formats offer unique advantages for addressing sexual loneliness through peer support, social skill practice, and normalization of relationship difficulties. Group interventions may include psychoeducational components about relationships, structured social skills practice, and process-oriented discussions about relationship experiences and goals. The group format provides opportunities to practice social interaction in a supportive environment while receiving feedback and encouragement from peers with similar experiences.
Psychodynamic approaches explore unconscious factors that may contribute to sexual loneliness, including defense mechanisms against intimacy, repetition of early relationship patterns, and internal conflicts about relationships. These interventions may be particularly valuable for individuals whose sexual loneliness reflects deeper psychological issues that require exploration and resolution before satisfying relationships can develop.
Integration of medical and psychiatric treatment may be necessary when sexual loneliness co-occurs with conditions that require medication management. Depression, anxiety disorders, ADHD, and other conditions may benefit from pharmacological intervention as part of comprehensive treatment planning. Medical evaluation may also identify hormonal or physical factors that contribute to sexual loneliness and require specific medical intervention.
Prevention and Public Health Strategies
Effective prevention of sexual loneliness requires comprehensive public health approaches that address societal factors contributing to relationship difficulties while promoting individual and community resilience. Prevention strategies must recognize the complex interplay between individual vulnerabilities and environmental factors that create risk for sexual loneliness, implementing interventions at multiple levels to maximize effectiveness.
Educational interventions represent fundamental prevention strategies that can be implemented across various settings and age groups. Relationship education programs should address realistic relationship expectations, communication skills development, conflict resolution strategies, and emotional regulation techniques that contribute to relationship success. These programs prove most effective when implemented before relationship difficulties develop, suggesting the importance of incorporating relationship education into school curricula, college programming, and community education initiatives.
School-based prevention programs should address social skills development, emotional intelligence, and healthy relationship concepts appropriate to developmental stages. Early intervention programs can help children and adolescents develop social competencies that reduce risk for later relationship difficulties. These programs should address topics including friendship formation, conflict resolution, emotional communication, and respect for others while promoting inclusive attitudes that reduce social isolation risk.
College and university prevention programs should address the specific relationship challenges faced by young adults transitioning to independence while managing academic and career pressures. Campus programming might include workshops on relationship skills, stress management, and balancing personal relationships with academic demands. Peer support programs and social activities that facilitate meaningful connections can help prevent social isolation during this critical developmental period.
Community-based prevention initiatives should focus on creating environments that facilitate relationship formation and maintenance while providing support for individuals experiencing relationship difficulties. Community programming might include social activities for various age groups, support groups for single individuals, and educational programs about relationship health. Faith-based organizations, community centers, and civic groups can play important roles in providing social connection opportunities.
Workplace interventions represent important prevention opportunities given the significant time adults spend in work environments. Employee assistance programs can provide relationship counseling and stress management resources that prevent relationship difficulties from escalating to sexual loneliness. Workplace policies that support work-life balance may help employees maintain relationships while managing career demands.
Mental health promotion strategies should address risk factors for sexual loneliness while building resilience and coping skills. Public awareness campaigns can reduce stigma associated with relationship difficulties and encourage help-seeking when problems arise. Mental health literacy programs can help individuals recognize signs of relationship distress and connect with appropriate resources.
Technology-based prevention approaches should address both the risks and benefits of digital technology for relationship development. Digital literacy programs can help individuals use technology effectively for relationship formation while avoiding pitfalls such as excessive choice options, unrealistic expectations, and reduced commitment. Guidelines for healthy technology use in relationships can help couples maintain connection while managing digital distractions.
Healthcare integration involves training healthcare providers to recognize and address sexual loneliness as a health concern. Primary care providers, mental health professionals, and specialists should understand the health implications of sexual loneliness and be prepared to provide appropriate referrals and interventions. Routine screening for relationship satisfaction and social connection can help identify individuals at risk for sexual loneliness.
Policy interventions may address structural factors that contribute to sexual loneliness, such as housing policies that facilitate community building, zoning regulations that promote walkable neighborhoods, and economic policies that support family formation. Urban planning that creates spaces for social interaction and community connection can help prevent social isolation that contributes to sexual loneliness.
Research and surveillance systems should monitor sexual loneliness prevalence and trends to guide prevention efforts and evaluate intervention effectiveness. Population-based surveys can track relationship patterns, satisfaction levels, and associated health outcomes. Research should identify protective factors and resilience indicators that can inform prevention program development.
Cultural interventions should address social norms and expectations that may contribute to sexual loneliness while promoting attitudes that support relationship formation and maintenance. Media literacy programs can help individuals critically evaluate relationship portrayals in media and develop realistic relationship expectations. Cultural messaging that emphasizes relationship skills development rather than simply relationship outcomes may promote healthier approaches to intimate connection.
Future Directions and Research Implications
The emerging recognition of sexual loneliness as a significant public health concern opens numerous avenues for future research that could substantially advance understanding and intervention effectiveness. Research priorities should address fundamental questions about etiology, prevalence, intervention efficacy, and prevention strategies while examining how sexual loneliness intersects with other health conditions and social phenomena.
Longitudinal research represents a critical need for understanding the developmental trajectories of sexual loneliness and identifying factors that predict onset, persistence, and resolution. Prospective studies following individuals from adolescence through various life stages could illuminate how early experiences, personality factors, and environmental influences shape sexual loneliness risk. Such research could identify critical intervention points and inform prevention program timing and content.
Intervention research should examine the comparative effectiveness of different therapeutic approaches for sexual loneliness, including individual therapy modalities, group interventions, and combined treatment approaches. Randomized controlled trials comparing cognitive-behavioral therapy, interpersonal therapy, acceptance-based interventions, and other approaches could guide evidence-based treatment selection. Research should also examine factors that predict treatment response and identify strategies for personalizing interventions based on individual characteristics.
Neurobiological research could advance understanding of the physiological mechanisms underlying sexual loneliness and its health consequences. Brain imaging studies examining neural activity patterns associated with sexual loneliness could illuminate how relationship absence affects brain function and emotional regulation. Hormonal studies could clarify how sexual loneliness affects stress hormone systems, reproductive hormones, and other biological markers.
Cultural and cross-cultural research should examine how sexual loneliness manifests across different cultural contexts and identify universal versus culture-specific aspects of the phenomenon. Comparative studies across cultures with different relationship norms, family structures, and social support systems could reveal protective factors and risk conditions. Such research could inform culturally adapted interventions and identify transferable prevention strategies.
Technology research should examine both positive and negative effects of digital technology on sexual loneliness while developing and testing technology-based interventions. Studies of dating applications, social media, and other digital platforms could identify design features that promote meaningful connection versus superficial interaction. Research should also examine the effectiveness of online therapy, mobile applications, and other technology-delivered interventions for sexual loneliness.
Gender and diversity research should examine how sexual loneliness affects different demographic groups while identifying factors that contribute to disparities in prevalence and outcomes. Research should examine sexual orientation differences, racial and ethnic patterns, socioeconomic influences, and other diversity factors that may affect sexual loneliness experiences. Intersectional approaches could illuminate how multiple identities interact to influence sexual loneliness risk and manifestation.
Prevention research should test and refine prevention programs while identifying optimal timing, intensity, and delivery methods. Studies should examine school-based programs, community interventions, and population-level approaches to preventing sexual loneliness. Cost-effectiveness research could guide resource allocation and policy decisions regarding prevention program implementation.
Economic research should quantify the societal costs of sexual loneliness, including healthcare utilization, productivity losses, and other economic impacts. Such research could strengthen the case for public health investment in prevention and intervention programs while informing policy decisions about resource allocation. Economic evaluation of interventions could guide evidence-based program selection and implementation.
Public health surveillance systems should be developed to monitor sexual loneliness prevalence and trends while tracking associated health outcomes. Regular population surveys incorporating sexual loneliness measures could provide data for policy planning and program evaluation. Surveillance systems should examine demographic patterns, geographic variations, and temporal trends to guide targeted interventions.
Conclusions and Clinical Implications
Sexual loneliness represents a complex, multifaceted public health challenge that requires sophisticated understanding and comprehensive intervention approaches. The evidence reviewed demonstrates that sexual loneliness extends far beyond temporary relationship absence to encompass profound effects on physical health, mental wellbeing, and overall life satisfaction. The increasing prevalence of sexual loneliness, particularly among young adults, combined with its significant health consequences, positions this phenomenon as a critical concern for healthcare providers, mental health professionals, and public health officials.
The clinical implications of sexual loneliness research are substantial and multifaceted. Healthcare providers must recognize sexual loneliness as a legitimate health concern that warrants clinical attention and appropriate intervention. Routine assessment of relationship satisfaction and intimate connection should be incorporated into comprehensive health evaluations, with particular attention to individuals presenting with depression, anxiety, or unexplained physical symptoms that might reflect underlying sexual loneliness.
Mental health professionals require specialized training to assess and treat sexual loneliness effectively. Traditional therapeutic approaches may need modification to address the unique aspects of sexual loneliness that differ from general loneliness or specific mental health conditions. Treatment planning should incorporate understanding of individual factors contributing to sexual loneliness while addressing both symptom relief and underlying relationship capacity development.
The prevention implications are equally significant, requiring coordinated efforts across multiple sectors and settings. Educational institutions, healthcare systems, community organizations, and policy makers must collaborate to create environments that support healthy relationship development while providing resources for individuals experiencing relationship difficulties. Prevention programs should begin early in development and continue across the lifespan, recognizing that sexual loneliness risk factors and manifestations change with age and life circumstances.
Public health approaches to sexual loneliness must address both individual and societal factors that contribute to relationship difficulties. While individual interventions focus on personal skills and psychological factors, broader approaches should examine social policies, cultural norms, and environmental factors that either facilitate or hinder intimate relationship formation and maintenance. The complex interplay between individual and societal factors requires coordinated intervention strategies that address multiple levels simultaneously.
The research implications highlight numerous opportunities for advancing understanding and intervention effectiveness. Future research should prioritize longitudinal studies, intervention trials, and prevention program evaluation while examining cultural variations and technological influences on sexual loneliness. Interdisciplinary collaboration between psychology, medicine, public health, sociology, and other fields will be essential for addressing the complex nature of sexual loneliness comprehensively.
Healthcare system implications include the need for integrated approaches that address sexual loneliness within broader health promotion and disease prevention frameworks. Healthcare providers should be trained to recognize sexual loneliness as a health risk factor and be prepared to provide appropriate referrals and basic interventions. Integration of relationship counseling and social support services within healthcare systems could improve accessibility and effectiveness of interventions.
The societal implications of sexual loneliness extend beyond individual suffering to encompass broader questions about social cohesion, community health, and cultural values regarding relationships and human connection. Addressing sexual loneliness effectively requires societal commitment to supporting intimate relationships and creating conditions that facilitate meaningful human connection. This may involve reconsidering cultural messages about relationships, examining social policies that affect relationship formation, and investing in community resources that bring people together.
In conclusion, sexual loneliness represents an emerging public health crisis that requires immediate attention and coordinated response across multiple domains. The evidence demonstrates clear relationships between sexual loneliness and various health outcomes, with particular concerns about increasing prevalence among young adults. Effective response requires integration of clinical intervention, prevention programming, research advancement, and societal commitment to supporting human connection and intimate relationship health. The urgency of this challenge, combined with the availability of evidence-based intervention approaches, creates both an opportunity and an imperative for comprehensive action to address sexual loneliness as a significant threat to individual and public health.
| Health Domain | Impact of Sexual Loneliness | Mechanisms | Intervention Targets |
| Cardiovascular Health | Increased risk of hypertension, coronary artery disease, stroke | Chronic stress activation, elevated cortisol, increased inflammation | Stress management, social support, relationship counseling |
| Mental Health | Higher rates of depression, anxiety, suicidal ideation | Reduced self-esteem, hopelessness, cognitive distortions | Cognitive-behavioral therapy, interpersonal therapy, mindfulness interventions |
| Immune Function | Decreased immune response, increased infection susceptibility | Chronic stress suppression, inflammatory markers | Stress reduction, social connection, lifestyle interventions |
| Sleep Quality | Disrupted sleep patterns, insomnia, poor sleep efficiency | Anxiety, rumination, absence of partner comfort | Sleep hygiene education, anxiety treatment, relaxation training |
| Pain Management | Increased pain sensitivity, reduced pain tolerance | Absence of natural comfort mechanisms, stress amplification | Pain coping strategies, social support, stress management |
| Demographic Group | Prevalence Patterns | Primary Manifestations | Targeted Interventions |
| Young Adult Men (18-24) | 30% report no sexual activity in past year | Complete sexual inactivity, anger, social withdrawal | Social skills training, confidence building, therapeutic support |
| Young Adult Women (18-24) | Lower rates of complete inactivity, higher relationship dissatisfaction | Quality concerns, emotional intimacy deficits | Communication skills, relationship expectations work |
| Middle-Aged Adults | Increasing prevalence within existing relationships | Partnership dissatisfaction, decreased intimacy | Couples therapy, relationship enrichment programs |
| Older Adults | Variable patterns based on partner loss, health status | Adjustment to loss, health-related barriers | Grief counseling, health management, social opportunities |
| Sexual Minorities | Higher rates due to limited partner pools | Identity integration challenges, social stigma | Affirmative therapy, community connection, identity support |
| Therapeutic Approach | Target Population | Primary Techniques | Expected Outcomes |
| Cognitive-Behavioral Therapy | Individuals with negative thought patterns | Cognitive restructuring, behavioral activation, exposure therapy | Improved mood, increased social engagement, realistic relationship expectations |
| Interpersonal Therapy | Those with relationship skill deficits | Communication training, interpersonal problem-solving | Enhanced relationship skills, improved social functioning |
| Acceptance and Commitment Therapy | Individuals struggling with acceptance | Values clarification, mindfulness, committed action | Increased life satisfaction, reduced avoidance behaviors |
| Group Therapy | Socially isolated individuals | Peer support, social skills practice, normalization | Reduced isolation, improved social confidence, peer connections |
| Couples Therapy | Partnered individuals with intimacy issues | Communication enhancement, intimacy building | Improved relationship satisfaction, enhanced intimate connection |
 sexmedclinic.com
sexmedclinic.com
